Tracking and fully applying the six pillars of lifestyle medicine at the clinical practice level is an administrative nightmare, says Canada’s Dr Jasdeep Saluja, or it was, until he and two colleagues got serious about using AI.
In an address to the ACLM’s 2025 conference, he explained what happened when his practice, Aroga Lifestyle Medicine, began “integrating artificial intelligence to restore time, clarity and connection” with the patients they serve.
It wasn’t a talk about gadgets or hype. It was a lived account of how their clinics, based in British Columbia and Ontario, are doing all they can to make lifestyle medicine tangible, scalable, and profoundly personal.
Along the way, he told health professionals attending, they discovered that AI, used carefully, could help return healthcare to what matters most: “the human being in front of us.”
Aroga Lifestyle Medicine was born in 2017, out of frustration and conviction. Saluja, alongside Dr Jesse Pewarchuk and Amar Magon, kept seeing a familiar pattern: patients leaving the clinic confused, overwhelmed, and unable to implement lifestyle changes that could literally save their lives. They wanted more than theory; they wanted to make lifestyle medicine real.
“Our role was founded on the mission to make lifestyle medicine tangible,” Saluja said, “not just theoretical advice, but practical, actionable guidance.” They believed patients should be partners, not passive recipients. Care had to be sustainable for patients, providers, and health systems.

But, in its fullest sense, lifestyle medicine is complex. It’s deeply personal and relentlessly detailed. It requires multidisciplinary collaboration and substantial documentation. Saluja painted a candid picture: an hour with a patient, followed by two hours documenting; a doctor, head down, typing relentlessly while a patient waited for connection.
Lifestyle medicine isn’t a quick prescription. It’s six pillars that demand nuance: nutrition, physical activity, sleep, stress, social connection, and avoidance of risky substances. Nutrition isn’t simply “eat better”—it’s culture, cooking skills, food access, and readiness. Exercise isn’t “move more”—it’s injuries, preferences, fears, barriers, and progression. Every visit meant pages of notes, instructions to allied health, customised resources, and intricate follow-up coordination. It was meaningful work, but it wasn’t scalable.
Group visits
The team turned to group medical visits. These provided community, connection, and shared momentum. Patients learned together. Providers could deliver care more efficiently. But building each program took months. The structure, the content, the facilitation—all of it was a heavy lift.
Simultaneously, the administrative reality felt like “organised chaos.” Manual scheduling across multiple providers, endless phone tag with patients and staff, insurance delays, coordinating group visits, preparing education materials—the constant burden fell on the clinic’s administrative backbone.
“If we don’t solve the administrative burden,” Saluja warned, “we’ll never be able to truly scale lifestyle medicine or reach the patients who need us most.”

Dr Jasdeep Saluja
Following a successful career as a hospital-based internal medicine doctor, Jasdeep has become an international thought leader on Lifestyle Medicine. He is a Diplomate of both the American Board of Lifestyle Medicine (ABLM) and the American Board of Obesity Medicine (ABOM). He is passionate about helping people lead the lives they love, and is a respected voice, serving on the Board of Directors for the ABLM since January 2020.
And there’s another truth that many clinicians rarely say aloud.
“The programs we developed took months on end,” he said. “This was me before—drowning in research papers, spending months for a single comprehensive lifestyle medicine program.”
He and his team manually reviewed articles and studies, parsed guidelines, assembled presentations—always high-quality, evidence-based material. But it wasn’t consistently engaging or interactive for patients. And it wasn’t scalable.
But with AI as copilot, everything changed.
Saluja now develops a comprehensive program in hours, not months. AI rapidly analyses thousands of research papers, identifies the most relevant evidence, and helps structure curricula grounded in behaviour change, coaching, psychology, and adult learning. The programs shifted from “information delivery” to “application design”—intentionally built to help patients integrate knowledge into daily life and see change from day one.
In just hours, AI generates core components: pre-reading, PowerPoint decks, follow-up handouts, and structured facilitator guides with key questions and discussion prompts. “AI creates an exceptionally strong foundation,” Saluja explained—“an amazing first draft backed by evidence, structured for impact, aligned to behaviour change theory.” From there, clinicians refine, validate, and elevate with their own training and lived experience. Clinicians lead and endorse every program. AI simply removes manual burden, freeing teams to focus on delivering the highest-quality care.
AI tools introduced
Aroga introduced AI tools over the past year to lighten administrative load: intelligent inbox management, automated chart creation, streamlined referrals, and direct integration of labs and documents into patient charts. These early steps reduced cognitive burden and gave staff breathing room.
But Saluja’s eyes were on the horizon. By year’s end, patients would be able to book appointments via an AI-assisted chat in the clinic’s app, guided to the right provider and appointment type based on their needs.
Long pre-visit questionnaires would become natural conversations instead of pages of forms. An AI-assisted triage system was underway. Decades of unstructured records—even 25-year stretches of PDFs—were being transformed into clean, usable clinical data.
“This isn’t simply about adding more technology,” he emphasised. “It’s about creating a more human experience, freeing our teams to do what only humans can do: connect, coordinate, and care.”
AI scribe impact
The most intimate transformation arrived through AI scribes. While the visit unfolded, the AI listened unobtrusively, analysing conversations in real time, capturing clinical details and lifestyle nuances that might otherwise be missed.
For Saluja, the effect was immediate: “Instead of typing with my head down while my patient’s speaking, I’m looking them in the eye. I’m listening deeply. I’m being fully present.”
Provider surveys told the same story:
- Time saved: 73% saved at least one full hour per day; 47% saved one to two hours.
- Connection restored: 100% reported more direct patient interaction time.
- Attention where it belongs: Every provider now spends 75–100% of the visit looking at the patient, not the computer.
Patients felt the difference. They felt heard, valued, and understood. Consent rates for AI scribe use reached 99%.
“When we use AI transparently, ethically, and clearly in service of care,” Saluja said, “patients don’t resist it. They trust it.”
The big bonus
Before AI scribes, patients often faced complex medical terminology, lengthy instructions, and murky next steps. Research shows patients forget much of what they’re told immediately after a visit. The AI scribe became a meaningful step in changing that. Patients now leave with clear, actionable summaries—in plain language, and in any language they prefer.
Instead of “reduce refined carbohydrates,” they see “swap bread for whole grain options you enjoy.” Instead of “increase physical activity,” they receive personalised progression guidance based on injuries, preferences, and barriers. Engagement rises. Adherence improves. Outcomes follow. When patients understand their plan and receive consistent support, they succeed.
Saluja cited evidence that AI-supported lifestyle medicine is not only promising—it’s transformational. In a randomised controlled trial with 150 patients with type 2 diabetes, the AI-supported lifestyle group achieved astonishing results: 71% reached an A1C below 6.5 compared to 2.4% in standard care; 8.6% average weight loss compared to 4.6% in usual care; and notable reductions in medication dependence.
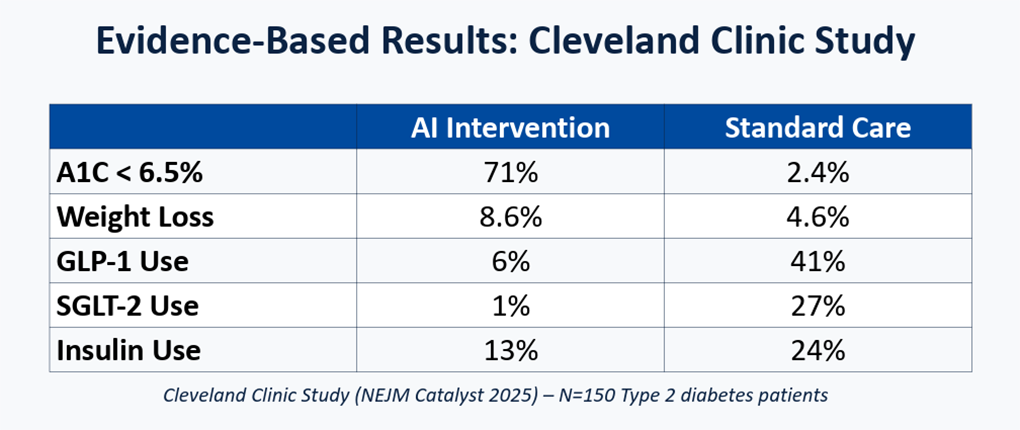
“These aren’t just statistics,” Saluja said. “They represent patients who moved from multiple medications to managing diabetes primarily through lifestyle change.”
The conclusion was clear: AI-powered lifestyle medicine works—and may work better than anything seen before.
The future vision
Saluja’s most exciting vision is for precision lifestyle medicine. Imagine not waiting for disease to declare itself, but identifying signals years before diabetes, heart disease, or metabolic dysfunction take hold. AI can analyse patterns across time, behaviour, and biology, detecting subtle shifts and convergence points that humans rarely catch in real time.
Personalisation will deepen interventions tailored not only to clinical observations, but also to genetic predisposition, microbiome composition, behavioural patterns, and social determinants of health.
“AI could evaluate your genetic risk for cardiovascular disease, your behavioural patterns around stress, sleep, eating, and exercise, and the impact of your social environment on daily choices,” Saluja said. “Then it could generate a lifestyle medicine plan that’s not only evidence-based, but precision-tailored to your unique biological and social profile.”
At the population level, AI will help identify community health trends and design interventions that address root causes—targeting systems, not just symptoms. The promise is prevention at scale: earlier, smarter, fairer.
Throughout his presentation, Saluja insisted on the human core.
“AI is handling the complexity—the thousands of data points no human can realistically process. Clinicians are free to focus on what we do best: human connection, empathy, and healing relationships.”
As he sees it, technology doesn’t replace the human element; it amplifies it. And he didn’t gloss over the risks.
The challenges
He cited five challenges head-on:
- Accuracy and reliability:
Reality: AI scribes and predictive algorithms are only as good as their training data, and errors can creep in.
Imperative: Clinician oversight is essential. Verification isn’t optional. - Algorithmic bias:
Reality: If training data underrepresents specific populations, systems can perpetuate disparities.
Imperative: Diverse datasets, bias audits, and equity-by-design are mandatory. - Privacy and security:
Reality: Healthcare involves sensitive data vulnerable to breaches and misuse.
Imperative: Robust safeguards, minimal necessary data use, and transparent practices. - Access and literacy:
Reality: Digital divides can exclude those who would benefit most.
Imperative: Multi-channel access, plain-language design, assisted support, and community partnerships. - Regulatory and ethical frameworks:
Reality: Without transparency, accountability, and patient trust, innovation stalls.
Imperative: Clear consent processes, explainable AI, outcome monitoring, and governance.
Acknowledging these challenges doesn’t weaken the case for AI—it strengthens it. Ethical innovation is not a box-tick but a discipline.
Reactive to predictive
Saluja framed the shift succinctly: AI is helping lifestyle medicine move from reactive to predictive care. “We’re not just treating disease. We’re beginning to prevent it,” he said. The evidence—from improved diabetes outcomes to sustained weight loss and reduced medication dependence—points to a consistent truth: the tools being adopted are transforming what’s possible.
Significantly, AI isn’t replacing the human element. It’s enhancing it. It’s giving back time, presence, and mental space. It’s helping clinicians focus on the person, not the screen; the story, not the checkbox.
The future of lifestyle medicine is more personal because AI handles data complexity; more precise because interventions align with each person’s biology and lived experience; and more powerful because evidence-based care can finally scale beyond the lucky few.
“The equation is simple,” Saluja concluded. “Technology plus humanity equals optimal patient outcomes.”
New programs
Dr Saluja described the new shape of programs emerging at Arogo:
- Application-first curricula:
Designed around behaviour change principles—implementation intentions, habit stacking, and motivational interviewing—so patients practice in-session and leave with micro-steps they can actually do. - Adaptive pathways:
Modules that adjust based on readiness, barriers, and preferences, offering beginner, intermediate, and advanced tracks without stigma. - Cultural and linguistic tailoring:
Material delivered in plain language and local contexts, with food and activity options grounded in culture, geography, and access. - Community scaffolding:
Facilitator guides prompt peer discussion, shared problem-solving, and social accountability—transforming knowledge into connection. - Outcome loops:
Built-in reflection points and feedback capture what’s working, informing updates to content and personal plans. AI summarises progress and flags needs; clinicians validate and adjust.
This isn’t about flashier slides. It’s about programs that move with people’s lives, that meet them where they are, and that turn health goals into daily practices.
The patient experience
Patients described three noticeable shifts:
- Clarity:
After visits, they receive concise summaries with concrete swaps, stepwise progression, and “next best action” tailored to their context—food preferences, injuries, schedules, and social environment. - Support:
Follow-ups feel timely and relevant, not generic. Reminders are conversational rather than prescriptive. Questions in the app are answered quickly, steering them to the right provider or resource. - Momentum:
Early wins matter. Programs start small—five-minute walks after dinner, high-fiber breakfast swaps, gentle wind-down routines—then stack into lasting change.
When care is understandable, responsive, and kind, self-efficacy grows. People do the work because it feels possible.
The clinician experience
Clinicians report three parallel shifts:
- Presence:
AI scribes carry documentation weight, enabling eye contact, curiosity, and deeper listening. Visits feel like conversations again. - Clarity:
Summaries are coherent and consistent. Allied health teams receive structured requests. Charts are easier to read. Fewer details slip through. - Collaboration:
Group programs are easier to spin up and iterate. Facilitators have shared guide rails. Cross-disciplinary care aligns around the patient’s plan rather than fragments of it.
Burnout is not solved by software. But reducing cognitive and clerical load frees space for the work that energises clinicians: connecting, problem-solving, teaching, and celebrating progress.
Pragmatic benefits
For health systems and clinics, AI-assisted workflows offer pragmatic benefits:
- Scale:
Programs that once took months to build now launch in days. Content can be localised and translated without starting from scratch. - Consistency:
Standardised summaries and facilitator guides reduce variation and drift, while leaving room for clinical judgment. - Equity:
Multilingual materials, plain-language design, and tiered digital support widen access—especially when paired with community delivery models. - Measurement:
Outcome loops—A1C changes, weight, sleep metrics, adherence markers—are easier to track and learn from, informing resource allocation and quality improvement.
Saluja says the aspiration isn’t to mechanise care. It’s to make good care easier to deliver, everywhere. He concluded with a practical, collective invitation.
- To healthcare providers:
“Explore AI tools for lifestyle medicine practice. You don’t have to wait for perfect solutions—start with pilot programs. Measure outcomes and iterate. Partner with technology companies, but choose those developing evidence-based solutions, not just flashy apps. Demand the same rigour in AI tools that you demand in clinical research.” - To patients:
“Ask your healthcare providers about AI solutions they’re using. If they’re not using any, ask them to look into it—and share what you’ve learned. You have more power than you think.” - To innovators and entrepreneurs:
“Collaborate with lifestyle medicine practitioners. Don’t build solutions in isolation. Address real clinical needs across the six pillars of lifestyle medicine. Focus on evidence-based solutions that improve outcomes, not just user engagement metrics.”
Together, he argued, we can create a future where precision lifestyle medicine is accessible to everyone—where technology amplifies human connection and where disease is prevented, not just treated.