Although still currently expensive, wearable technology looks set to reshape and enhance the delivery of lifestyle medicine, Dr Lara Zakaria, told LM2025 this morning. Her presentation, From Behaviour to Longevity: Using Wearable Tech to Personalise Lifestyle Medicine, challenged clinicians and patients alike to rethink how we measure, interpret, and act on health data.
She said the era of one-size-fits-all nutrition and wellness is ending: technology is opening the door to truly individualised care.
Zakaria began by grounding her audience in sobering statistics. According to the CDC, 60% of Americans live with at least one chronic disease, and these conditions account for 86% of healthcare costs.
This epidemic is not only unsustainable but also deeply tied to lifestyle factors—diet, sleep, stress, and physical activity. For Zakaria, the solution lies in moving beyond generic guidelines toward precision interventions that reflect each person’s unique biology.
Central to her argument was the concept of “food as medicine.” Zakaria highlighted bioactive compounds such as sulforaphane (from cruciferous vegetables), EGCG (green tea catechins), resveratrol (grape skins), curcumin (turmeric), and quercetin (onions and apples).
Pathway influencers
These compounds influence pathways such as glutathione production, NF-κB signalling, and oestrogen metabolism—mechanisms that regulate inflammation, detoxification, and resilience against oxidative stress. In other words, what we eat can directly modulate the molecular systems that drive chronic disease.
Yet, as she noted, nutrigenomic outcomes depend on a dynamic interplay of genetics, microbiome, environment, and lifestyle. The same food can yield vastly different results depending on the individual. This variability underscores the need for personalised nutrition strategies.
Zakaria outlined the challenges in scaling personalised nutrition. Traditional tools—food diaries, frequency questionnaires, and static lab values—fail to capture real-time metabolic responses. Clinicians often lack actionable data, while patients face overwhelming streams of information from wearables and apps. Without proper interpretation, this flood of numbers can lead to anxiety or misapplication.
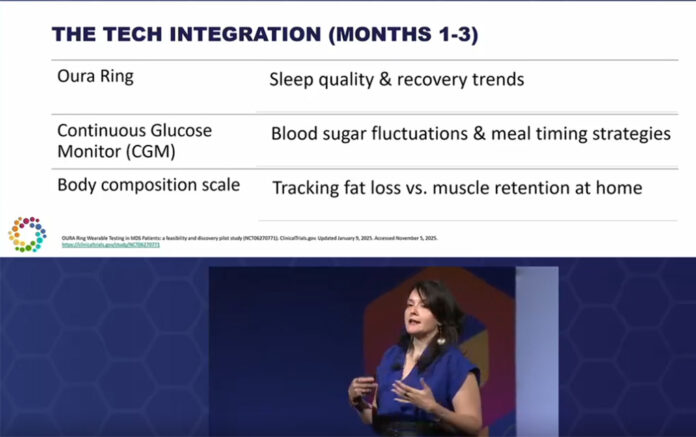
Still, she argued, wearable technology offers a way forward. Devices like continuous glucose monitors (CGMs), Oura Rings, and smart scales provide real-time feedback on how diet, sleep, and activity affect metabolism. When integrated thoughtfully, these tools empower patients to make adaptive choices and clinicians to tailor interventions with unprecedented precision.
Case study: Sam’s journey
To illustrate, Zakaria shared the story of “Sam,” a 44-year-old woman struggling with weight loss resistance. Despite foundational lifestyle changes, Sam plateaued at a BMI of 30. Lab findings revealed hormonal imbalances, low adrenal reserve, and signs of leptin resistance. Rather than prescribing another static diet plan, Zakaria integrated wearable data into Sam’s care.
- Oura Ring tracked sleep quality and recovery, revealing inconsistent patterns that impacted stress resilience.
- CGM monitoring identified post-meal glucose spikes and overnight dips, guiding adjustments in carbohydrate timing and protein intake.
- Smart scales monitored shifts in body composition, distinguishing fat loss from muscle retention.
Within three months, Sam lost eight pounds, reduced visceral fat, and increased muscle mass. More importantly, she gained metabolic flexibility—the ability to switch efficiently between burning carbohydrates and fats. This adaptability, Zakaria emphasised, is the cornerstone of long-term health and energy stability.
While the technology is promising, Dr Zakaria cautioned against over-reliance. Wearables cannot track everything, and data silos make integration into clinical practice cumbersome. Privacy concerns, device fatigue, and obsessive tracking are real risks. She urged clinicians to balance data with intuition, listening to patients’ lived experiences rather than reducing health to metrics alone.
Pragmatic takeaways
Her takeaways were pragmatic:
- Focus on long-term trends, not daily fluctuations.
- Use wearable insights to fine-tune diet, exercise, and rest.
- Choose devices that align with patient goals rather than chasing novelty.
- Engage patients in interpreting data, ensuring it empowers rather than overwhelms.
Zakaria also addressed the growing use of GLP-1 receptor agonists for weight loss. While effective at reducing fat mass, these drugs can drive significant muscle loss—up to 40–60% of total weight lost. Muscle, she reminded the audience, is metabolically active tissue essential for glucose regulation, strength, and independence in ageing. Losing it accelerates frailty, cognitive decline, and metabolic dysfunction. Wearables that track body composition, therefore, are critical for ensuring weight loss strategies preserve lean mass.
For wearable tech to fulfil its promise, she argued, healthcare systems must evolve. Clinician-facing dashboards that consolidate data across devices, integrate with electronic health records, and allow real-time trend analysis are urgently needed. Until then, practitioners must navigate fragmented platforms, adding complexity to already time-constrained workflows.
A call for enrichment
This presentation was not a call to abandon traditional medicine but to enrich it with personalised, data-driven insights. Wearables, when used wisely, can transform lifestyle medicine from reactive to proactive, helping patients sustain behaviour change and optimise health outcomes. But the technology is only as powerful as the human relationships guiding its use.
Her final message resonated: health technology offers opportunity, but it must be balanced with intuition, empathy, and patient-centred care. Personalised nutrition works best when adaptive, responsive, and grounded in both science and lived experience.
For Whole Food Living readers, the takeaway is inspiring: the future of wellness is not about chasing numbers but about harnessing them to tell a deeper story of resilience, longevity, and human potential.