Lifestyle medicine (LM) has moved from the margins of healthcare into the centre of urgent conversations about chronic disease, cost, and sustainability, American College of Lifestyle Medicine President Dr Padmaja Patel, told the LM2025 conference earlier today.
The latest updates from AACLM highlight both the progress made and the challenges ahead as the field seeks to scale its impact, influence policy, and secure its place in mainstream healthcare.
But despite remarkable technological advances, healthcare outcomes remain stubbornly poor, she said. Rising costs, declining patient satisfaction, and the relentless burden of chronic disease—heart disease, diabetes, and obesity—signal a system under strain.
Progress feels stalled because innovation has not been matched with whole-person care. Lifestyle medicine offers that missing link, focusing on prevention, reversal, and patient empowerment rather than fragmented disease management.
Patients increasingly demand proactive, sustainable solutions. Yet clinicians often lack training in lifestyle interventions, leaving a gap between evidence and practice. LM addresses this by centring care around six pillars: optimal nutrition, physical activity, restorative sleep, stress management, connectedness, and avoidance of risky substances. These interventions are not fringe recommendations—they are embedded in clinical guidelines for many chronic conditions as first‑line treatments.
Clinical practice
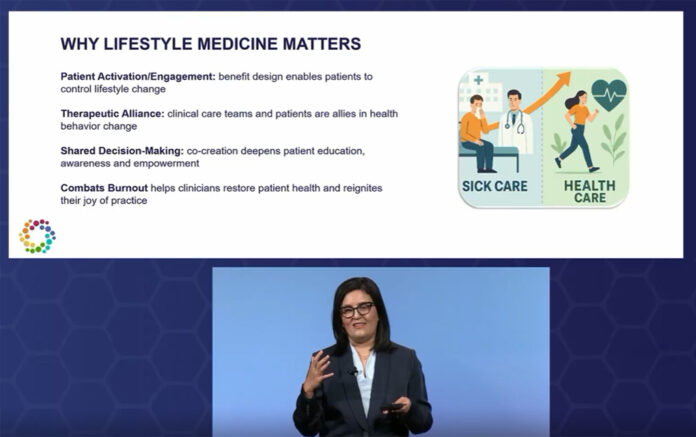
Traditional care models emphasise diagnosis, prescription, and clinician responsibility. LM reframes this dynamic: patients become active partners, care is team‑based, and education and motivation replace passive treatment.
Medication may still play a role, but the emphasis shifts toward remission and prevention. This transformation not only restores patient health but also combats clinician burnout by reigniting the joy of practice.
ACLM has invested heavily in research projects such as the LEADR (Lifestyle Empowerment Approach for Diabetes Remission) pilot, deprescribing studies, and validation of dietary screening tools. Position papers on intensive therapeutic lifestyle change, planetary health, and obesity guidelines further strengthen the evidence base.
Education is expanding rapidly: residency programs in LM have grown from just seven in 2018 to nearly 475 in 2025, preparing the next generation of clinicians to integrate lifestyle interventions into practice.
Policy and payment reform
One of the most significant developments is the alignment of LM with federal policy. The Centers for Medicare & Medicaid Services (CMS) Innovation Center has recognized LM’s role in prevention and health restoration.
New coding advancements, such as ICD‑10 updates for documenting diabetes remission, and recharacterisation of HCPCS codes to emphasise lifestyle assessment, signal a shift toward valuing LM interventions.
Payment reform is also underway, with hybrid models and team‑based approaches designed to reward outcomes like medication de‑escalation and disease remission rather than perpetuating chronic disease management.
ACLM’s induction into the American Medical Association (AMA) House of Delegates marked a milestone in credibility, Dr Patel said. Its first clinical practice guideline—focused on lifestyle interventions for type 2 diabetes and prediabetes—sets a precedent for evidence-based LM integration.
Partnerships with Epic to embed LM assessment tools into electronic health records further mainstream the practice. Platinum partnerships with mission‑aligned organisations demonstrate that LM is not just a clinical movement but a systemic one.
Community engagement
Membership now spans 95 countries, with strong representation in the United States, Canada, Saudi Arabia, and the UAE. Interest groups in medical schools and health systems continue to grow, advocating for curriculum reform and contributing to research.
Podcasts like Flip Your Script and Next Gen LM extend the conversation, inspiring clinicians and patients alike to reimagine healthcare through lifestyle change.
She said the roadmap for 2026 emphasises financially sustainable LM interventions, expanded state‑level advocacy, and scaling of the Diabetes Remission Project. By operationalising clinical models, building robust research repositories, and aligning payment and quality measures, LM aims to secure its role as the foundation of value‑based care.
“Lifestyle medicine stands at a crossroads. The evidence is clear, the demand is rising, and policy is beginning to catch up.”
What remains is the collective will to scale Lifestyle Medicine across diverse care settings and populations. Success would decisively shift healthcare from disease management to health restoration—an outcome that benefits patients, clinicians, and society alike.